Psychiatric Follow Up Note Template
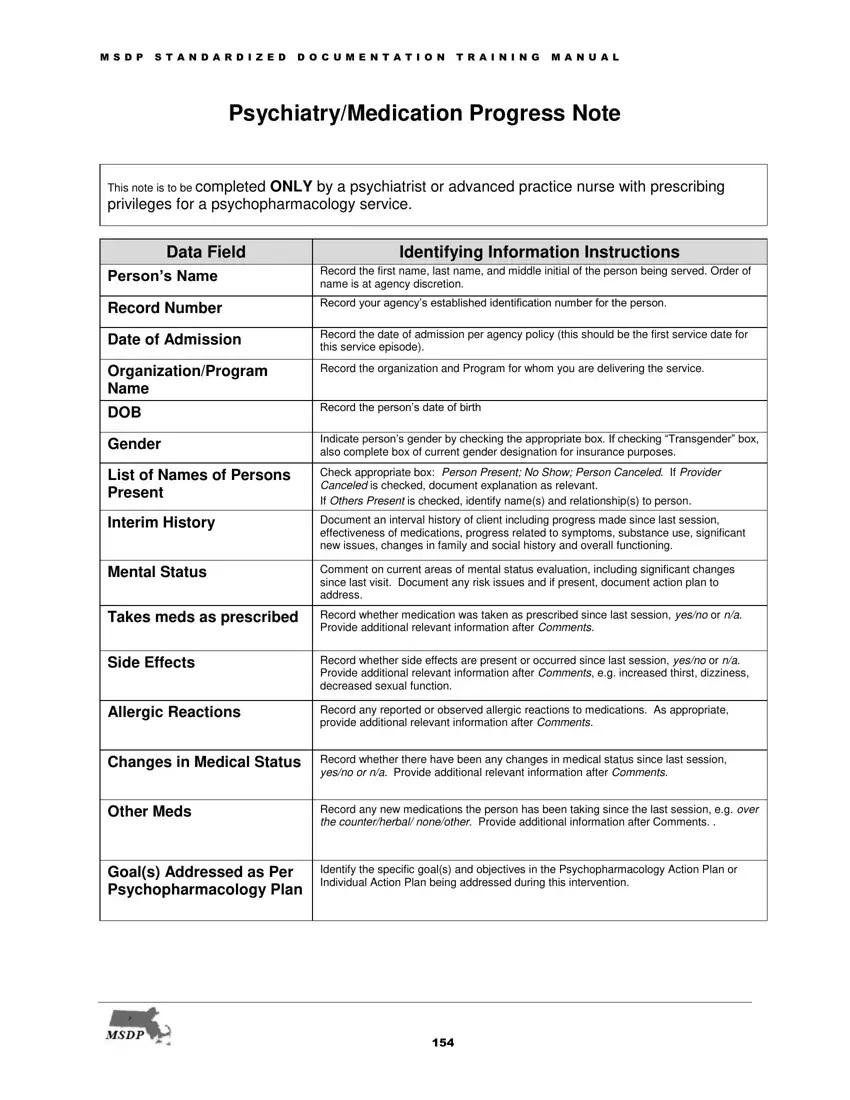
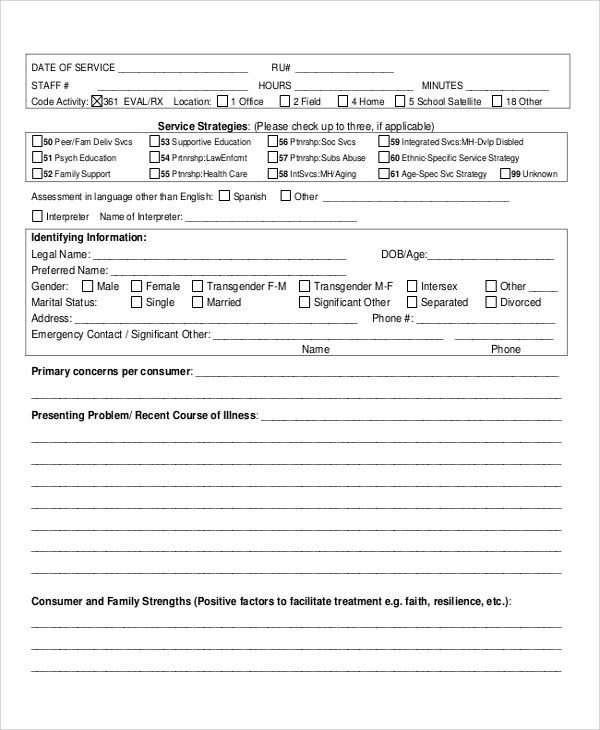
Psychiatric Follow Up Note Template - Web learn how to write therapy progress notes to document the details of every session. If you need these documents in a different format please contact andy benjamin, jd, phd, abpp. Delirium management on the consult service; For psychiatrists, nurse practitioners, nurses, physician assistants, residents, and students. Web psychiatry progress note templates to streamline your practice. Web psychiatric outpatient initial/followup note. Web soap notes can be a real pain in the brain. Not loose / obsessive / preoccupied / disorganized / personalized / circumstantial / tangential / blocking / somatic. Download our free therapy progress notes templates. “i am having less stress” hpi: “i am having less stress” hpi: Let mentalyc ai write your progress notes fast. Soap note template and example. 24 y/o hx of gad and mdd. The soap (subjective, objective, assessment, and plan) format is commonly used in medical documentation and includes information about the patient's symptoms, a mental status examination, an assessment of the patient's. Have the most common mental status exams ready to paste or include into your notes. She is currently prescribed the following psychotropic medications: Not loose / obsessive / preoccupied / disorganized / personalized / circumstantial / tangential / blocking / somatic. Psychiatry intake notes are connected to appointments when psychiatry intake is selected as the appointment type. X, a 56. This form is to be completed only by psychiatrist or advanced practice nurse with prescribing privileges when providing a service which includes psychopharmacology (the code name includes the terms evaluation and management) and psychotherapy. Web outpatient/office psychiatric progress note counseling and/or coordination of care (99214 or 99215) patient’s name: Have the most common mental status exams ready to paste or. But writing effective psych notes doesn't have to drive you up a wall. Web here are 15 examples you can use. If you need these documents in a different format please contact andy benjamin, jd, phd, abpp. The soap (subjective, objective, assessment, and plan) format is commonly used in medical documentation and includes information about the patient's symptoms, a mental. Web learn how to write therapy progress notes to document the details of every session. Web soap notes can be a real pain in the brain. Not sad / anxious / apathetic / worried / angry / labile / blunted / happy. 24 y/o hx of gad and mdd. Initial psychiatric evaluation note template. The soap (subjective, objective, assessment, and plan) format is commonly used in medical documentation and includes information about the patient's symptoms, a mental status examination, an assessment of the patient's. For psychiatrists, nurse practitioners, nurses, physician assistants, residents, and students. Lem ed grades are good (associated signs and symptoms) but patient appears distracted (quality) in class (context). Web outpatient/office psychiatric. Download our free therapy progress notes templates. Soap, dap, emdr, intake notes and more. *chief complaint* date and time of service: Web therapynotes' psychiatry intake note template allows you to capture both a robust biopsychosocial history of your patient and effectively document medical services within a single note. Approximately 224 views in the last month. Not sad / anxious / apathetic / worried / angry / labile / blunted / happy. “i am having less stress” hpi: Web psychiatric outpatient initial/followup note. Web following a template is an easy way to ensure all important details and information are included in your therapy progress notes. Abilify 15 mg, 1 tab po q day, fluoxetine hydrochloride 20. Used in appointments following the initial consultation, it provides a structured format for documenting a patient's progress, observations, and any changes in treatment or diagnosis. Web psychiatry progress note templates to streamline your practice. Web here are 15 examples you can use. No auditory or visual hallucinations. Not sad / anxious / apathetic / worried / angry / labile /. Approximately 224 views in the last month. Psychiatry progress note templates to streamline your practice. Soap, dap, emdr, intake notes and more. Needs to go to work soon, no issues with medications, hydroxyzine “helps” stressors (medical/family/relationship/financial/employment/educational/housing): For psychiatrists, nurse practitioners, nurses, physician assistants, residents, and students. The following is the hpi from one of their sample clinic notes: Approximately 224 views in the last month. Psychiatry intake notes are connected to appointments when psychiatry intake is selected as the appointment type. Web the miss usa who gave up her crown and title this week accused the pageant’s ceo of failing to take an incident of sexual harassment seriously and creating a toxic work environment, according to. Delirium management on the consult service; X, a 56 yowf with a history of paranoid schizophrenia and major depressive disorder, presents to the clinic for f/u. No auditory or visual hallucinations. “i am having less stress” hpi: Recording, dictation, text & upload inputs. This form is to be completed only by psychiatrist or advanced practice nurse with prescribing privileges when providing a service which includes psychopharmacology (the code name includes the terms evaluation and management) and psychotherapy. Web some of the common useful templates for psychiatry include basic inpatient admission orders (in “the plan”); *chief complaint* date and time of service: But writing effective psych notes doesn't have to drive you up a wall. Web learn how to write therapy progress notes to document the details of every session. Provide thorough coverage of your patient’s report on how their symptoms are responding to treatment. Documents are in microsoft word (.docx) format.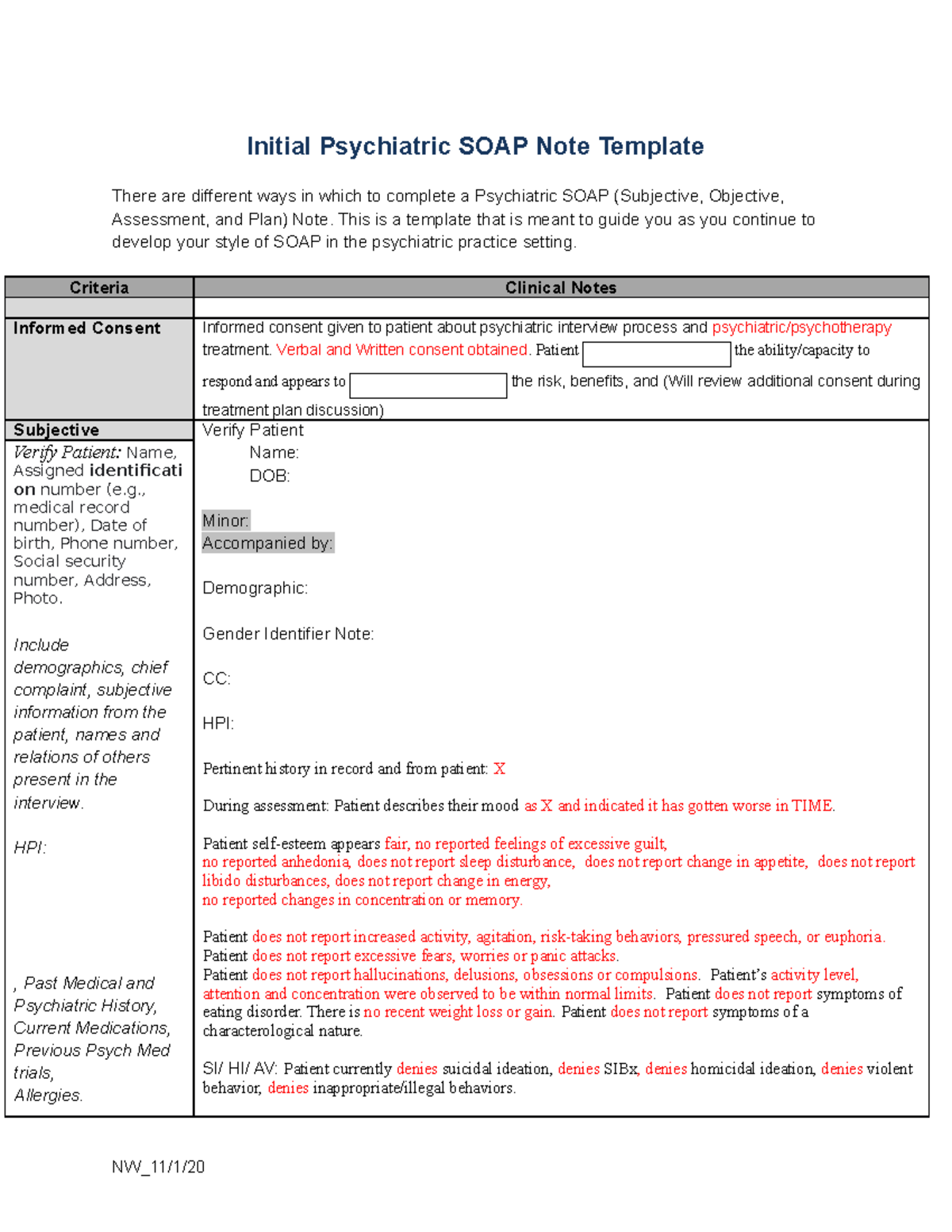
Soap Notes Template Mental Health

Psychiatric Progress Note Template

Psychiatric Follow Up Note Template May 19, 2022 Psych Team.Printable

Psychiatry Progress Note Template & Example Free PDF Download
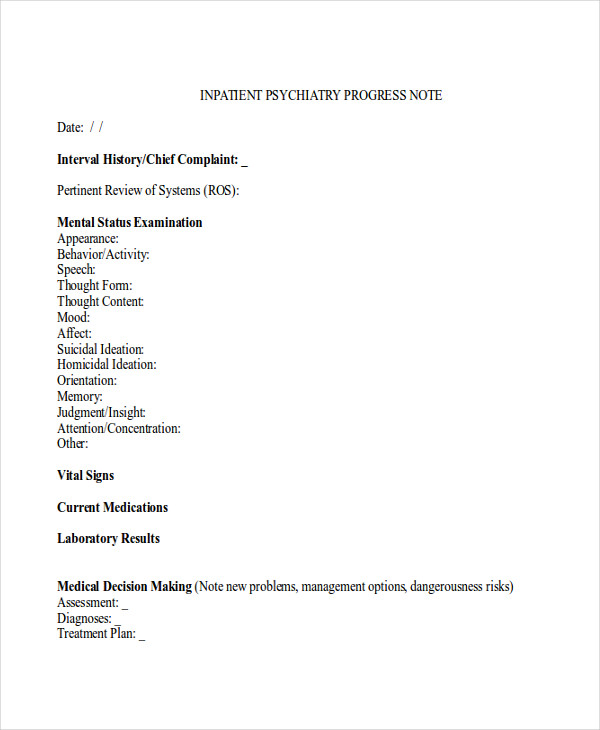
Psychiatric Progress Note Template
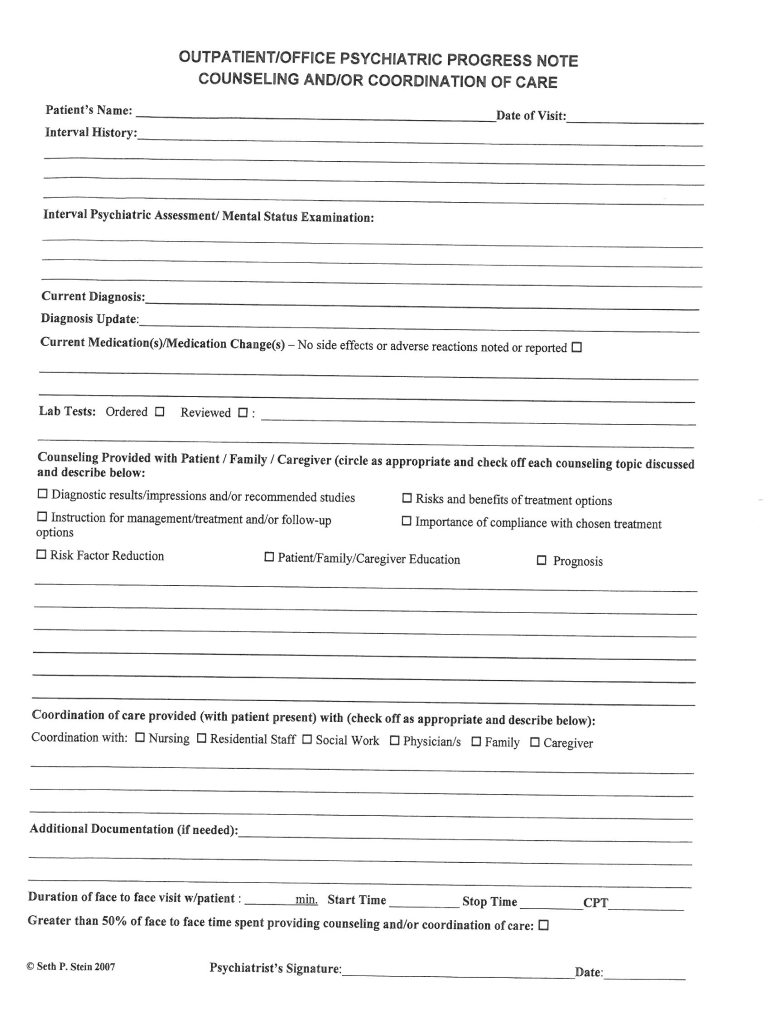
Outpatient/Office Psychiatric Progress Note Counseling and/or

Mental health progress note templates & examples (2023) Carepatron
Psychiatric Progress Note ≡ Fill Out Printable PDF Forms Online

Psychiatry Note Template
Comprehensive Psychiatric Evaluation Template
Web Outpatient/Office Psychiatric Progress Note Counseling And/Or Coordination Of Care (99214 Or 99215) Patient’s Name:
Have The Most Common Mental Status Exams Ready To Paste Or Include Into Your Notes.
The Soap (Subjective, Objective, Assessment, And Plan) Format Is Commonly Used In Medical Documentation And Includes Information About The Patient's Symptoms, A Mental Status Examination, An Assessment Of The Patient's.
Try It Out For Free.
Related Post: