Psych Soap Note Template
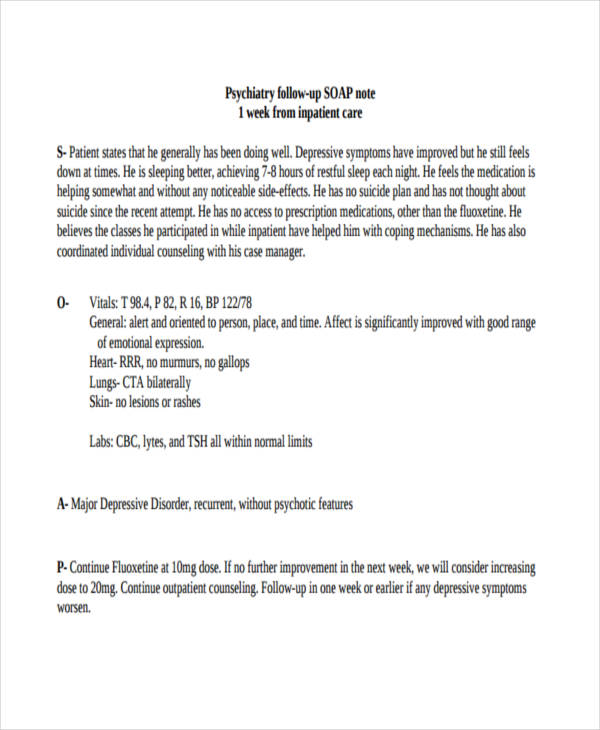
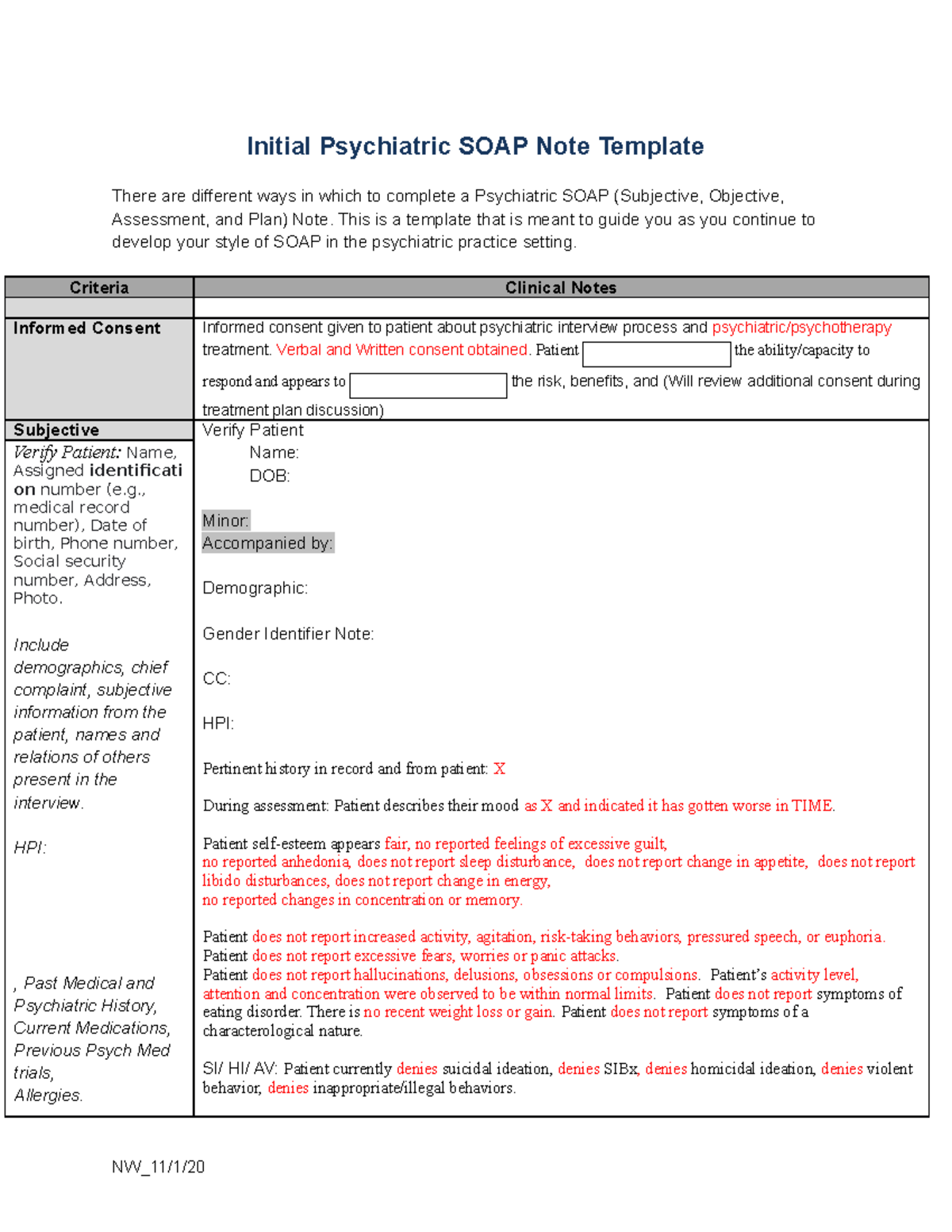
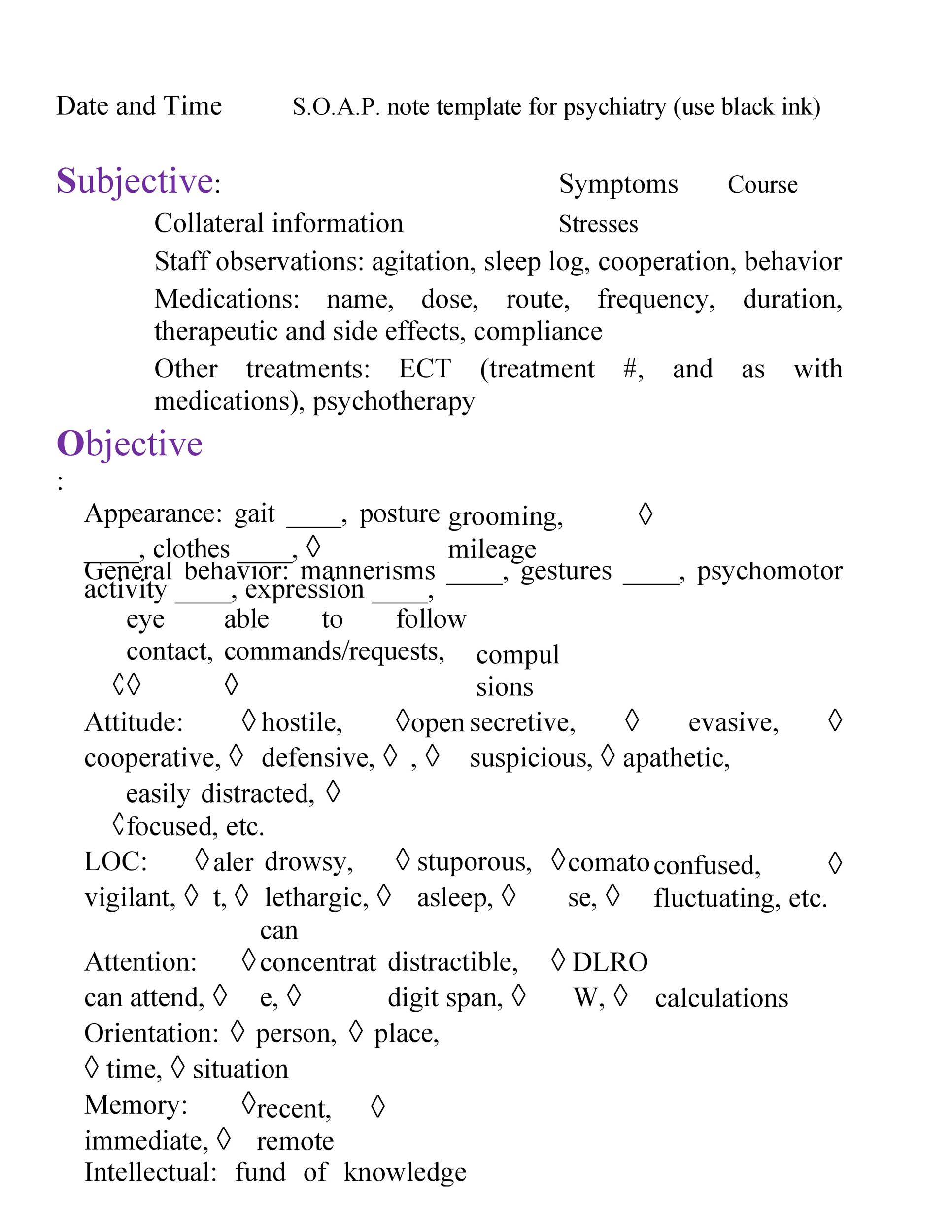
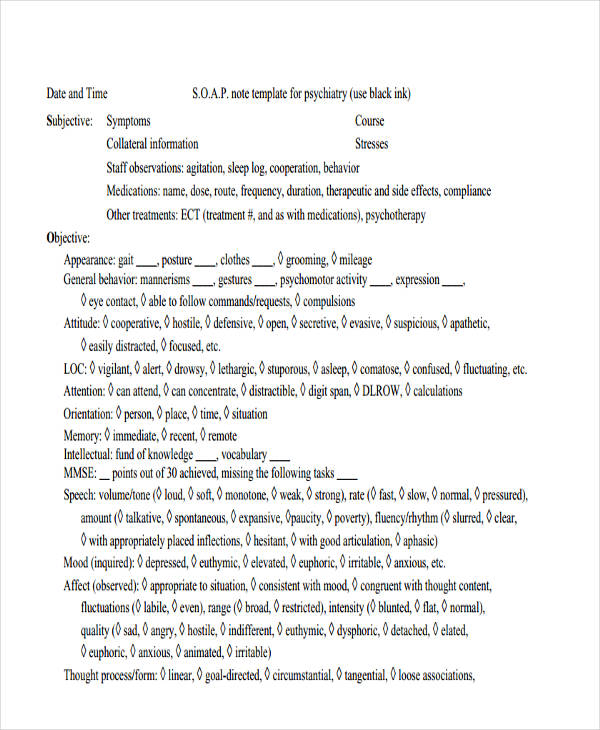
Psych Soap Note Template - Web information written in present tense, as appropriate. Structured data index 1, 19 form elements, 79 boilerplate words, 19 drop. The subjective section is where you document what your client is. Keeping track of clinical information for future reference and for the reference of future psychiatric/medical providers. Web soap note example for psychiatry. Soap notes offer concrete, clear language and avoid the use of professional jargon. Soap notes can be used by many different providers across different medical disciplines, but for our purposes. She reports feeling empty and worthless for the past several months, with worsening symptoms in the past two weeks. Notes that are organized, concise, and reflect the application of professional knowledge. Web how to write soap notes. Notes that are organized, concise, and reflect the application of professional knowledge. Web psychiatry note example #1. Keeping track of clinical information for future reference and for the reference of future psychiatric/medical providers. This guide provides a thorough overview of soap notes, their purpose, and essential elements tailored for pmhnps. This is a template that is meant to guide you. Soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. Soap notes are a helpful method of documentation designed to assist medical and mental health professionals in streamlining their clinical notes. Having an easy to use soap note like our editable pdf soap notes. The subjective section is where you document what your client is. Web soap notes help a private practice by providing organization, clarity, and a framework for clinical reasoning”. Mild, moderate, severe, psychotic features, in partial remission, in full remission etc.) data contained in the subjective and objective sections. Decreased verbal fluency noted on assessment—difficulty naming objects and generating lists. Web. As you sit down to write a soap note, reflect on your session and allow the four sections of the note template to guide you to document the most important aspects of your client’s current state and the progression of your treatment. Soap notes are extremely helpful in counseling. They deny suicidal thoughts or ideation. Mental health providers will find. This guide provides a thorough overview of soap notes, their purpose, and essential elements tailored for pmhnps. Used in appointments following the initial consultation, it provides a structured format for documenting a patient's progress, observations, and any changes in treatment or diagnosis. 5+ psychiatric soap note examples 1. Web read the entire article to know more about psychiatric soap notes. Possible mild cognitive impairment or early dementia. Mary jones, md (pcp) history: They include descriptions using the five senses. The soap note is often the most common for psychiatrists’ visits. Patient is currently assessed to be at risk for self harm or harm to others as evidenced by ideation and behavior on today's exam. Used in appointments following the initial consultation, it provides a structured format for documenting a patient's progress, observations, and any changes in treatment or diagnosis. Soap notes can be used by many different providers across different medical disciplines, but for our purposes. Web assessment diagnosis diagnosis: Denies nightmares or separation issues. Break information into digestible sections: Adhering to the standard soap format (subjective, objective, assessment, plan) ensures that your notes are easy to read and understand. The soap note is often the most common for psychiatrists’ visits. Web information written in present tense, as appropriate. Web a psychiatry progress note template serves as a standardized tool for psychiatrists. Break information into digestible sections: Divide the content into clear sections and use subheadings to further organize the information. They deny suicidal thoughts or ideation. Web they deny obsessive thoughts or ritualistic behaviors. The subjective section is where you document what your client is. This guide provides a thorough overview of soap notes, their purpose, and essential elements tailored for pmhnps. Soap notes are extremely helpful in counseling. How to write soap notes (examples & best practices) | sondermind You probably already know this, but soap is. Make sure that you take down notes for data gathering. Web how to write soap notes. Notes that are organized, concise, and reflect the application of professional knowledge. “i’ve been having panic attacks out of nowhere, and it’s scary.”. Use template to save time and to focus on the content quality. Web soap notes help a private practice by providing organization, clarity, and a framework for clinical reasoning”. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Using a template such as soap notes means that you can capture, store, and interpret your client's information consistently over time. They report eating meals per day and sleeping hours per night. Possible mild cognitive impairment or early dementia. Patient is currently assessed to be at risk for self harm or harm to others as evidenced by ideation and behavior on today's exam. Major depressive disorder with suicidal ideation: Web read the entire article to know more about psychiatric soap notes and how to create one. How to write soap notes (examples & best practices) | sondermind 5+ psychiatric soap note examples 1. This is a template that is meant to guide you as you continue to develop your style of soap in the psychiatric practice setting. Approximately 154 views in the last month. Web psychiatry note example #1..png)
SOAP Notes for Therapy Template & Example Free PDF Download
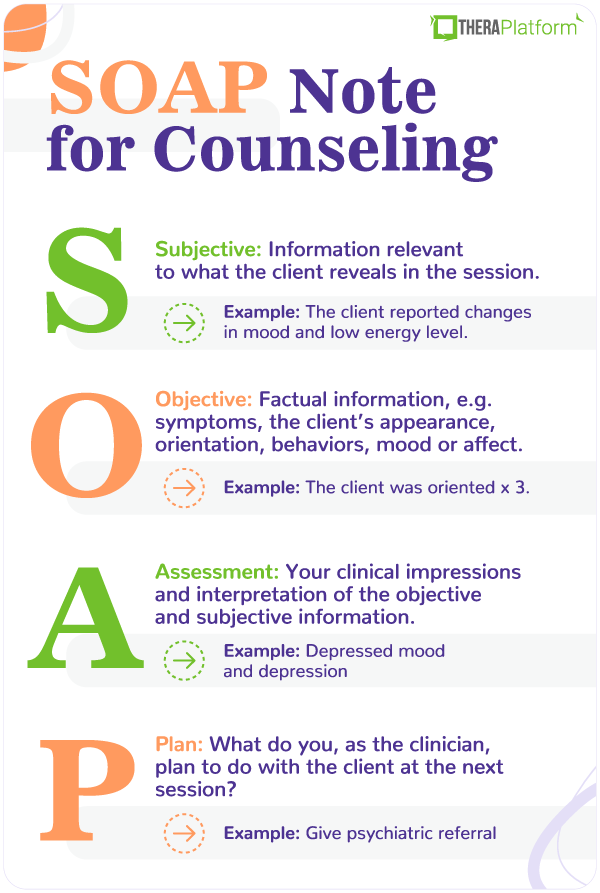
Soap Notes Template Counseling
Soap Note Template 34 PDF Psychotherapy Mental Health
SOAP Note Examples 19+ in PDF Examples
Soap Notes Template Mental Health
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
![]()
Tips for Writing Better Mental Health SOAP Notes [Updated 2021]

Counseling Progress Notes Template

Soap Notes Template Mental Health
SOAP Note Examples 19+ in PDF Examples
Structured Data Index 1, 19 Form Elements, 79 Boilerplate Words, 19 Drop.
Having An Easy To Use Soap Note Like Our Editable Pdf Soap Notes Allow Practitioners To Easily Store Client And Patient Notes, Organized By Each Session That They Attend.
They Deny Suicidal Thoughts Or Ideation.
Web Learn About Soap Notes And The Benefits They Provide In Capturing Important Information During Therapy Sessions.
Related Post:
