Patient Note Template
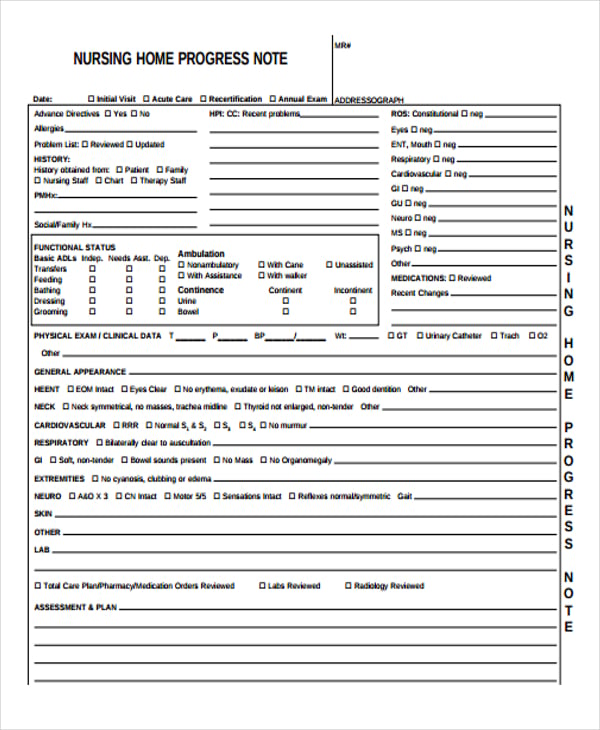
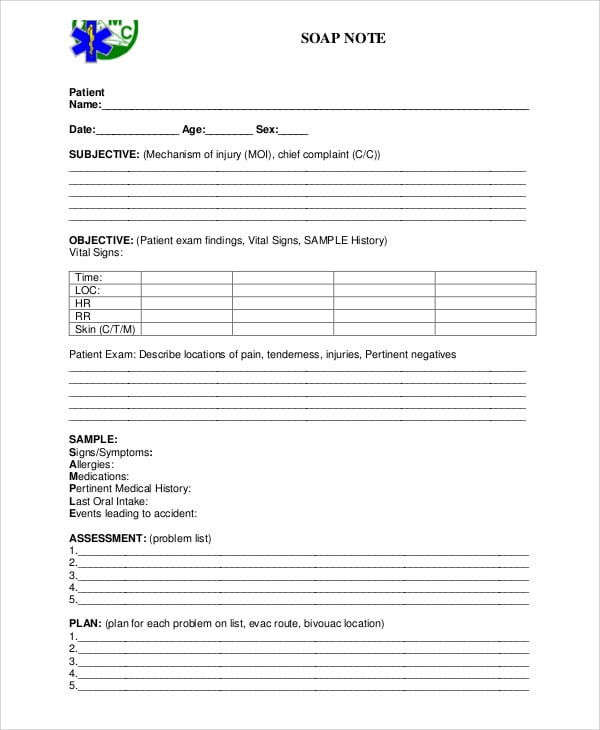
Patient Note Template - When patients are experiencing doubt or appear to be uneasy, mills encourages them to seek a second opinion. Soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. Subjective data, objective data, assessment data, and a plan of care. Web soap notes can be a real pain in the brain. Web what are patient progress notes? In the course of your duties, you take notes on every interaction you have with patients. Understanding and effectively utilizing soap notes is essential. It is the documentation used to record information about encounters with patients that follows a specific format. Web this toolkit will help you and your team address common clinician concerns and provide guidance on best practices for sharing clinical notes with patients. This structured documentation method is crucial for tracking patient progress and facilitating clear communication among healthcare professionals. Soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. The note text is always the same every time you use that template. Nurses, doctors, physical therapists, and all other members of the healthcare team who provide care to the patient will document notes in the patient’s chart. In. In the course of your duties, you take notes on every interaction you have with patients. Cardiology demands precise and comprehensive documentation for effective patient care. Soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. Web health professionals must have an accurate record of their patients. Web soap. Check out the example of a patient note, as well as a sample pdf so you can better understand the note within a health context. This structured documentation method is crucial for tracking patient progress and facilitating clear communication among healthcare professionals. Web this toolkit will help you and your team address common clinician concerns and provide guidance on best. Patient symptoms, treatment plans, medications are documented in nursing notes to ensure continuity and quality of care. Notes from your verbal interaction with patients as well as what they tell you about their condition go here. These notes are very important as you are usually the one who administers drugs to patients in the hospital. Web nursing note templates and. In this article, we'll walk you through the soap method, provide examples of solid psychiatry notes, give some proven tips to optimize your time — and throw a technological bone your way. Patient symptoms, treatment plans, medications are documented in nursing notes to ensure continuity and quality of care. A patient note within an ehr is the primary communication tool. Web nursing note templates and examples. Nursing notes are written records that document patient care and serve as a communication tool among healthcare professionals. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Subjective data, objective data, assessment data, and a plan of care. It is the documentation used. Patient progress notes are used to keep a record of a patient’s care when they are staying at a hospital. In the course of your duties, you take notes on every interaction you have with patients. This structured documentation method is crucial for tracking patient progress and facilitating clear communication among healthcare professionals. An intake assessment, treatment plan, and progress. Generate reports from completed checklists. 30 useful nursing note samples (+templates) october 28, 2020 6 mins read. In this article, we'll walk you through the soap method, provide examples of solid psychiatry notes, give some proven tips to optimize your time — and throw a technological bone your way. It is the documentation used to record information about encounters with. Web how clinical note templates work. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Eliminate paperwork with digital checklists. In the course of your duties, you take notes on every interaction you have with patients. Web 3 essential types of clinical documentation. Web soap notes can be a real pain in the brain. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Soap notes include four elements: Web how clinical note templates work. Generate reports from completed checklists. Cardiology demands precise and comprehensive documentation for effective patient care. It is part of a medical document where medical professionals record vital information such as the clinical standing of a certain patient during the time of confinement or during an outpatient assistance. Web soap note templates. Mills often sees patients who are coming to her for one, and she. As a nurse, you are one of the front liners in medical emergencies. This covers your patient’s detailed medical history and current symptoms. Soap notes include four elements: In the course of your duties, you take notes on every interaction you have with patients. Check out the example of a patient note, as well as a sample pdf so you can better understand the note within a health context. Helpful hints and tips within the templates can improve patient care and save time. Soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. How to write the perfect physical therapy soap note + examples and templates. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). When patients are experiencing doubt or appear to be uneasy, mills encourages them to seek a second opinion. An intake assessment, treatment plan, and progress notes. Web our note templates provide blocks of patient documentation that can be inserted into any note in any emr.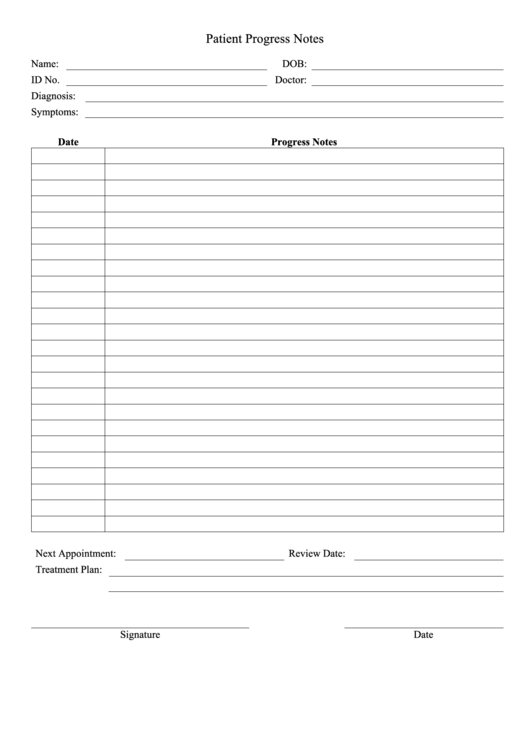
Free Printable Medical Progress Notes Printable Templates
.png)
Patient Note Template & Example Free PDF Download
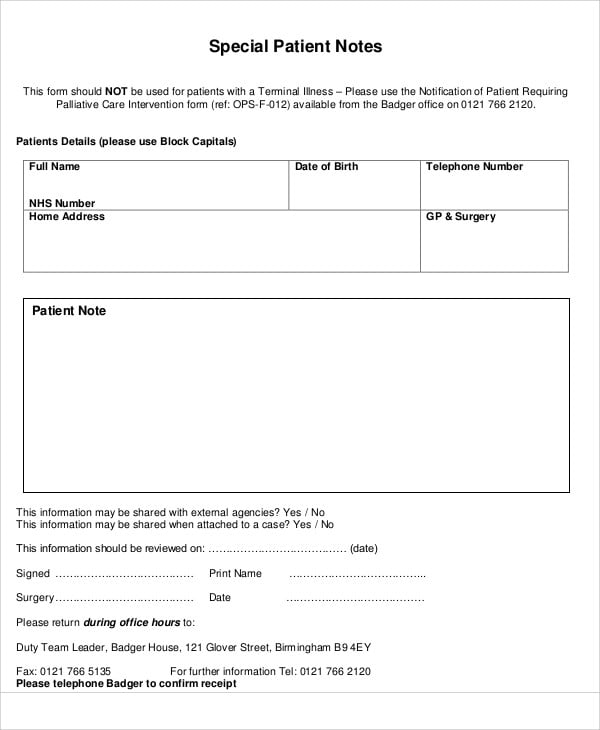
Patient Note Templates 7+ Free Samples, Examples Format Download

WORD of Medical Progress Note.docx WPS Free Templates

Clinical Notes Template
Patient Progress Notes Template Word
Patient Note Templates 7+ Free Samples, Examples Format Download

Patient Note Template Templates at
Patient Note Templates 7+ Free Samples, Examples Format Download
Patient Progress Notes Template Word
Notes From Your Verbal Interaction With Patients As Well As What They Tell You About Their Condition Go Here.
Web A Soap ( S Ubjective, O Bjective, A Ssessment, P Lan) Note Is A Method Of Documentation Used Specifically By Healthcare Providers.
Record Your Patient’s Chief Complaint, Existing Symptoms, And Any Pain Description In This Section.
Not Only Does It Protect Our Patients From Harm, But Documentation Also Protects Our.
Related Post: